The Challenge: Provide a Better Experience for Patients, Providers, and StaffOrgan transplantation is an incredible gift, but the complexity and uncertainty associated with the transplant evaluation process can be stressful for patients and families. Potential donors and recipients need to undergo extensive testing in multiple hospital departments to determine if they're a match, and the process of moving between various appointments throughout the hospital can create anxiety and inconvenience for patients, providers, and staff.
With the goal of creating a better and more streamlined experience for everyone involved in the crucial and life-giving process of organ transplantation, University of Wisconsin Hospital and Clinics engaged Flad to lead the design effort for a new clinic, hospital entry, and supporting spaces in partnership with UW Health Planning, Design and Construction. By consolidating a wide range of transplant services and innovative research, the project will help shape the future of comprehensive transplant patient and living donor care services.
The project provides a new home for UW Health's world-class transplant program, which was previously located in the lower level, by moving it to a prominent location on the main floor at the hospital's front door. The new clinic's design improves access and expands clinical space, reducing the need for patients to travel within the hospital for tests and other supporting services. Improved technology, a comfortable family lounge, dedicated education space, and other patient-centered features enhance the patient and family experience throughout all stages of transplant care.
A Data-Driven Approach to Transplant Center Design
The Challenge: Provide a Better Experience for Patients, Providers, and StaffOrgan transplantation is an incredible gift, but the complexity and uncertainty associated with the transplant evaluation process can be stressful for patients and families. Potential donors and recipients need to undergo extensive testing in multiple hospital departments to determine if they're a match, and the process of moving between various appointments throughout the hospital can create anxiety and inconvenience for patients, providers, and staff.
With the goal of creating a better and more streamlined experience for everyone involved in the crucial and life-giving process of organ transplantation, University of Wisconsin Hospital and Clinics engaged Flad to lead the design effort for a new clinic, hospital entry, and supporting spaces in partnership with UW Health Planning, Design and Construction. By consolidating a wide range of transplant services and innovative research, the project will help shape the future of comprehensive transplant patient and living donor care services.
The project provides a new home for UW Health's world-class transplant program, which was previously located in the lower level, by moving it to a prominent location on the main floor at the hospital's front door. The new clinic's design improves access and expands clinical space, reducing the need for patients to travel within the hospital for tests and other supporting services. Improved technology, a comfortable family lounge, dedicated education space, and other patient-centered features enhance the patient and family experience throughout all stages of transplant care.
The shared project vision was to "provide the best patient, provider, and staff experience and remain one of the top transplant programs in the country." Guiding principles included:
- Patient & Family Centered Care
- Comprehensive Care
- Identity & Image
- Culture & Community
- Innovation & Transformation
To ensure highest and best use of space, Flad implemented a combination of qualitative and quantitative approaches to collect and analyze data throughout the programming, planning, and design processes. We provided customized analytical tools to help determine future volumes, work toward improved operational processes, help users understand spatial flows, and ultimately deliver a successful outcome for the client.
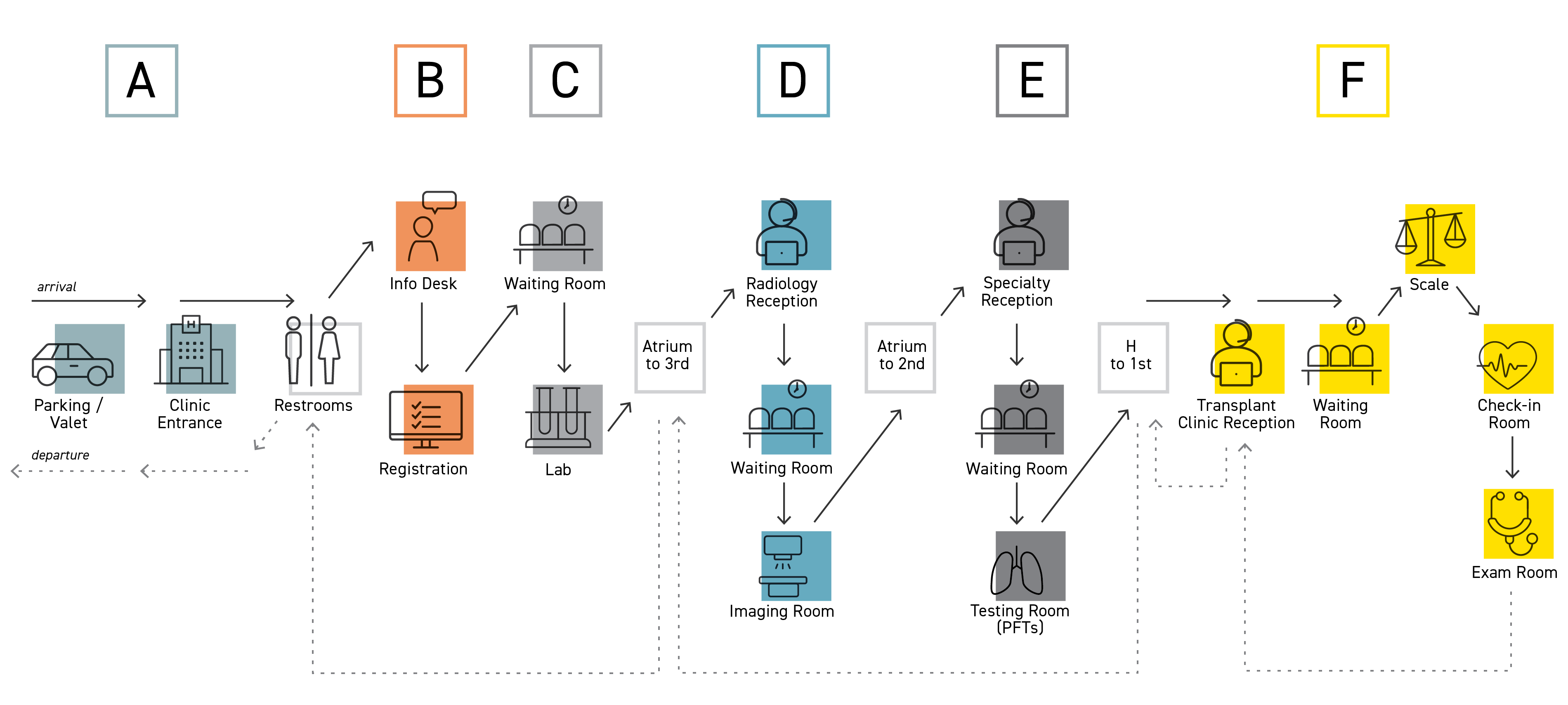
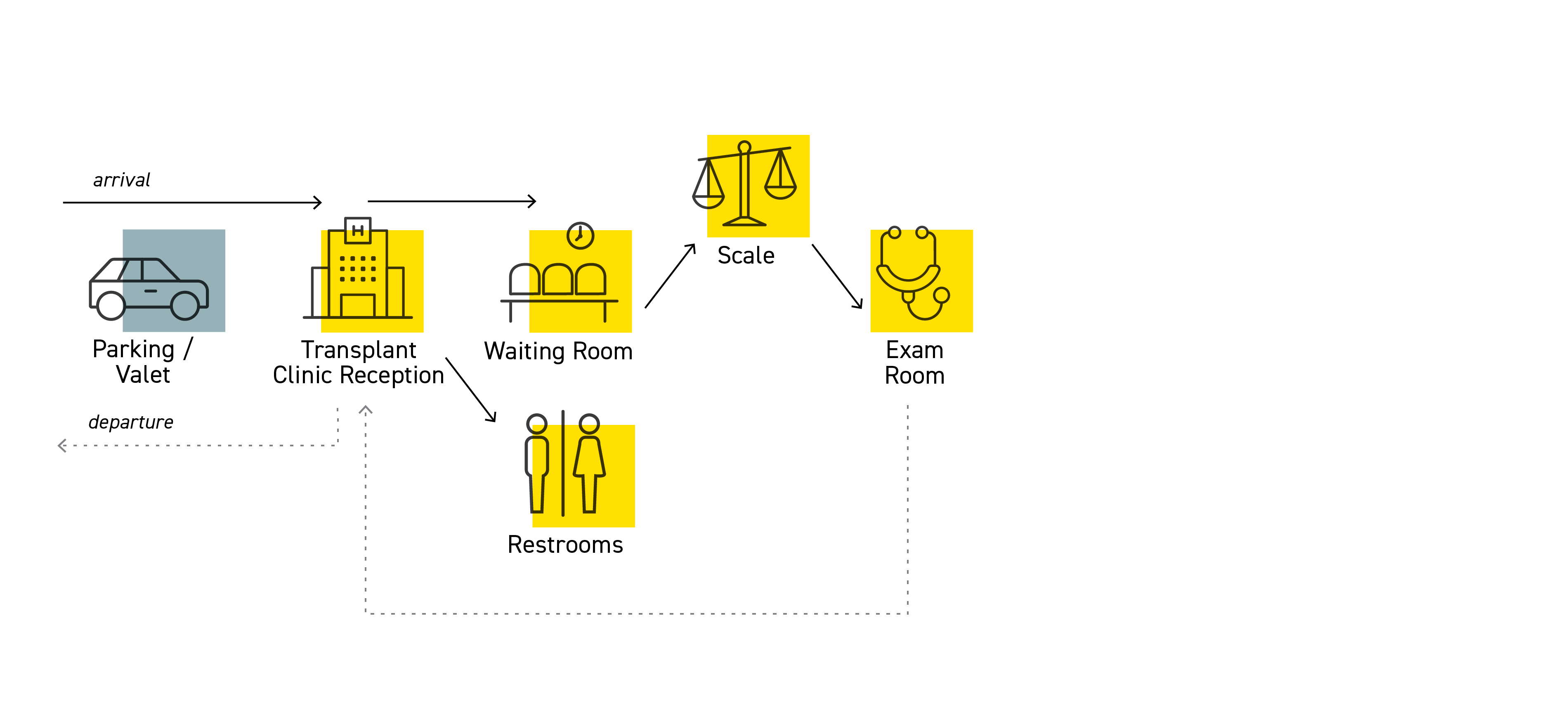
Patient-Centered, Flexible DesignOne of the project's primary goals was to improve the patient experience by consolidating services that are currently provided across multiple locations throughout the hospital. In the current state, many patients and family members walk long distances to access these services. Because the transplant program serves living donors and patients across various organ programs, space types in the new transplant center need to be flexible and accommodate a range of functions including procedures, infusions, post-transplant exam visits, multidisciplinary patient evaluations, specialty consults, patient education, lab draws, telehealth, and provider workspaces.
We took these steps to better understand the current state and develop the ideal future state:
1) Shadowing, Observations, and Process Maps. The design team spent several days on site, observing and shadowing clinicians and patients to understand current state workflows. We documented workflows using high-level process maps from the patient perspective, and shadowing helped us validate quantitative data on visit durations.
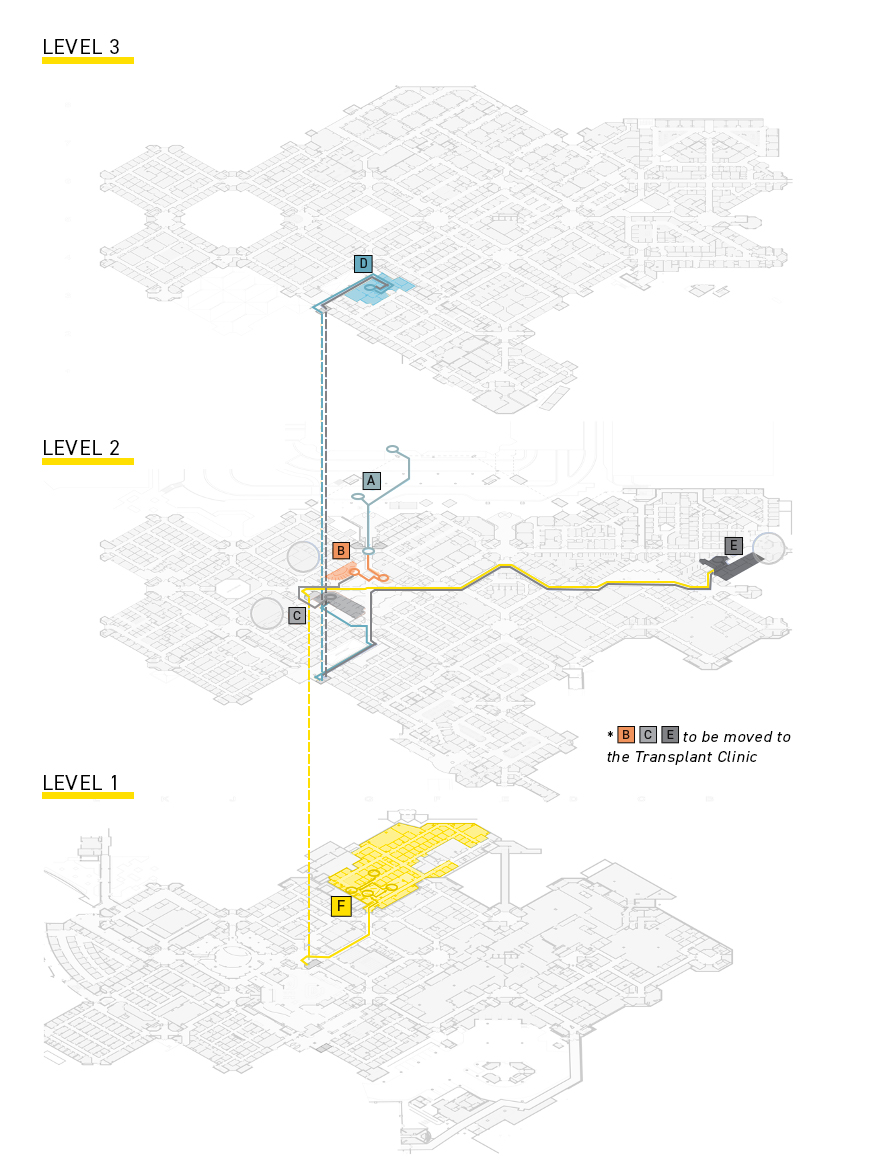
2) Axonometric Diagrams. We developed axonometric diagrams based on organ program and visit type to show the travel paths that patients are required to take in the current state. These diagrams allowed us to calculate approximate travel distances and provide visual aids to help decision-makers understand the current state and patient experience.
3) Surveys and User Sessions. After we attained an understanding of the current state, we held a series of workshops with key stakeholder groups to walk through the current state data, brainstorm opportunities for improvement, and start visualizing the ideal future state. We engaged patient and family advisors to provide the direct patient perspective.
4) Animations. The ideal state flows informed the new design of the clinic and support spaces. We developed animations to demonstrate the patient experience and arrival flow.
Service Growth ProjectionsAnother major goal was to accommodate anticipated future growth and new technology through flexibility in design. The transplant program has recently undergone substantial growth, and new clinical programs are slated for expansion. Space types have evolved significantly and are expected to continue to change.
Utilization Calculator and Scenario Modeling. We used modeling tools to project future patient volumes based on the transplant program's strategic plan, the organ program's business plans, new physician hires, and patient expectations then generated scenarios to understand the volume and space impacts of future growth rates.
Telehealth Modeling. Initial visit volume assumptions were revisited after the onset of the pandemic to incorporate the increased use of telehealth to deliver care. One of the silver linings of the pandemic, the increase in number of virtual visits, allowed the clinic design to focus on spaces required to optimize the patient experience for functions that must occur in person.
Bifurcated Operational Model Due to the limited space available on the entry floor level, Flad pursued a stacked, two-story option with patient spaces on the main floor and staff spaces, including ten telehealth rooms, on the floor below.
Tools used to help stakeholders visualize how services may be consolidated and future-state flows operationalized included the following:
Operational Process Mapping. We used a series of visual tools to communicate staff, patient, and equipment flows throughout the two floors. Process maps helped the team rethink current operations to create a feasible bifurcated model.
Block Diagrams and Axonometric Diagrams. Visual block diagrams showed program needs by space type compared to the available footprint on each floor. Interactive discussions with users allowed them to understand the benefits and tradeoffs of optimizing the patient experience by placing various space types on each level and thus how the bifurcated model could be operationalized.
The Result: Data-Driven Decisions Create a Streamlined ExperienceWhen implementing substantial changes in limited space, we've found that data-driven tools and approaches help all stakeholders stay focused on project goals and making the highest and best use of space. In this case, documenting patient travel times and distances, modeling future growth, and conducting other quantitative analyses contributed to a successful planning and design process. The hospital's new transplant center is currently under construction and is expected to open in late 2022. Part of Flad's design process involves post-occupancy evaluations; these will be conducted in 2023 and further analysis and results will be shared at that time.
Learn more about Flad's data-driven approach to healthcare settings